Pulmonary Physiology
Return to the Main Menu
Case 1:
(Click here to go to the answers)
A 44-year-old man awakens his wife in the middle of the night. She hears, "uuuhhh...uuuhhh...uuuhhh," a terrible gasping sound. This has happened irregularly for the past 5 years. The onset is typically without warning. She reaches for a medication which, when administered, alleviates his symptoms.
A routine checkup by his physician the next day reveals no abnormal findings.
Laboratory studies show: hematocrit 45%, glucose 80 mg/dL, and creatinine 1.1 mg/dL. An arterial blood gas on room air shows: pO2 95 mm Hg, pCO2 40 mm Hg, pH 7.41, HCO3 27 meq/L, and oxygen saturation 95%.
Questions:
1.1 What physical examination findings are most likely present during one of his episodes? What would a chest roentgenogram show?
1.2 What is the most likely diagnosis?
1.3 What is the medication he was given?
1.4 What long-term medication(s) would be indicated?
1.5 What are long-term sequelae of his disease?
Case 2:
(Click here to go to the answers)
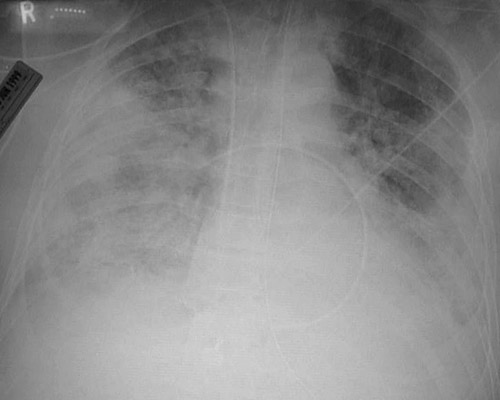
A 23-year-old man suddenly collapses to the ground while practicing tai-kwan-do. He is taken to the emergency department. Vital signs show T 36.9 C, P 88/min, RR 30/min, and BP 110/70 mm Hg. Auscultation of the chest reveals absent breath sounds on the right. There is tympany on the right. His heart rate is regular with no murmurs. No other significant findings are noted.
An arterial blood gas shows pO2 55 mm Hg, pCO2 30 mm Hg, pH 7.45, and HCO3 28 meq/L. After administration of 100% oxygen by nasal canula at 2 L/min, a repeat blood gas shows pO2 55 mm Hg, pCO2 30 mm Hg, pH 7.45, and HCO3 27 meq/L
A chest radiograph is taken.

Questions:
2.1 What was the sudden event?
2.2 Name conditions that may have predisposed to this event.
2.3 Explain the blood gas findings.
Case 3:
(Click here to go to the answers)
A 23-year-old woman has the sudden onset of dyspnea. She is taken to the emergency department. On examination vital signs show T 37 C, P 100/min, RR 25/min, and BP 100/70 mm Hg. Her lungs are clear to auscultation and no murmurs are heard. An electrocardiogram shows T-wave inversion in leads V1 to V4.
Laboratory findings show Hgb 14.2 g/dL, Hct 42.8%, MCV 91 fL, WBC count 7790/microliter, and platelet count 191,200/microliter. Her D-dimer is 5 (normal <0.5 miccrogram/mL). An arterial blood gas on room air shows pO2 95 mm Hg, pCO2 32 mm Hg, pH 7.46, and HCO3 23 meq/L.
Questions:
3.1 What is your differential diagnosis list?
3.2 What diagnostic studies may be done?
Example 1:
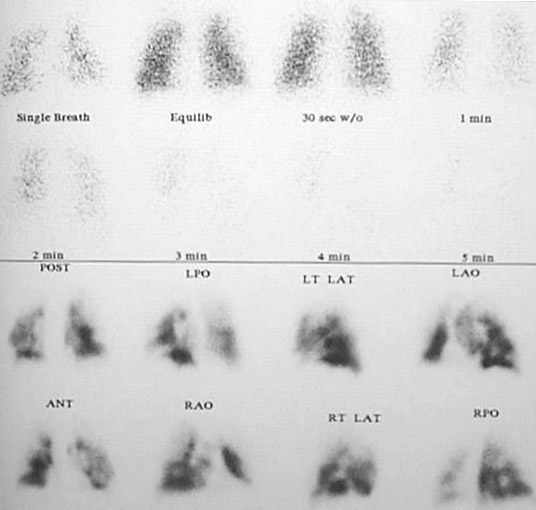
Example 2:

3.3 What additional studies are indicated?
Subsequent studies show:
| Lupus anticoagulant | negative
| | Prothrombin gene mutation | negative
| | Factor V Leiden mutation | positive
| | Protein C | normal
| | Protein S | normal
| | Antithrombin III | normal
| | Homocysteine | normal
|
3.4 What do these findings suggest?
Case 4:
(Click here to go to the answers)
A 74-year-old man has experienced substernal chest pain for the past 3 hours. The pain is constant. He is now becoming short of breath. In the emergency department his vital signs include temperature 37.1 C, pulse 108/min, respiratory rate 29/min, and blood pressure 90/70 mm Hg. He is unable to lie supine. Auscultation of the chest reveals bilateral crackles in lower lung fields. He has a summation (S3 and S4) gallop. A chest radiograph shows prominent bilateral perihilar infiltrates.
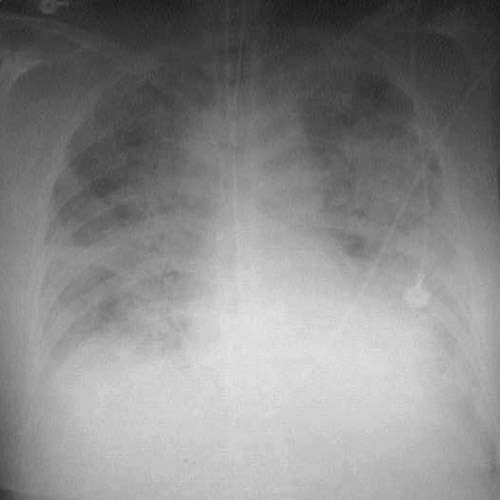
Example 1:

Example 2:
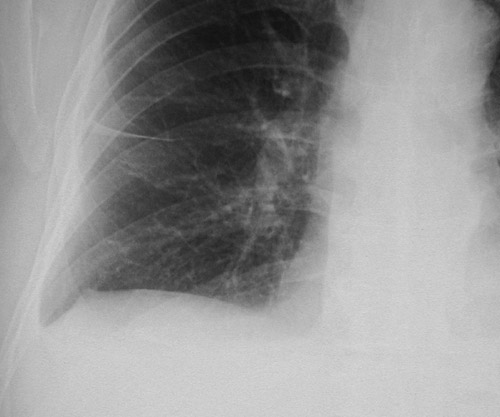
Example 3:
Questions:
4.1 What is suggested by these findings?
4.2 What tests would help confirm the diagnosis?
Additional history:
He is admitted to the hospital. He receives thrombolytic therapy with tPA. His condition is stable. He receives pharmacologic therapy with an anticoagulant, probably a low moleculart weight heparin analogue. Other possible therapies include an anti-platelet agent or a beta-blocker.
He now has the following hemodynamic pressures:
| Arterial BP | 100/75 mm Hg
| | RA (CVP) | 12 mm Hg
| | PA | 36/28 mm Hg
| | PAWP | 28 mm Hg
| | HR | 115/min
|
4.3 What do these findings indicate?
4.4 If his left chamber volume at end of diastole = 0.11 L, chamber volume at end of systole = 0.08 L, and he is an average-sized person with a body surface area of 1.62 m2, calculate his cardiac output, cardiac index, and ejection fraction.
Case 5:
(Click here to go to the answers)
A 48-year-old woman has had increasing dyspnea with exertion for the past 5 months. She has had a cough with copious sputum production for the past 3 months. She has smoked 1 to 2 packs of cigarettes per day for the past 30 years. On physical examination her vital signs include temperature 37 C, pulse 83/min, respiratory rate 23/min, and blood pressure 135/90 mm Hg. Auscultation of the lungs reveals scattered crackles in lung bases.
Questions:
5.1 What do these findings indicate?
5.2 What additional studies are indicated?
Pulmonary function testing reveals the following results:
| Parameter | Predicted | Observed
| | FVC(L) | 5 | 4
| | FEV1 (L) | 4 | 2
| | FEV1/FVC(%) | 80 | 50
| | MVV(L/Min) | 100 | 60
| | TLC(L) | 6 | 7
| | DLC0(ml/min/mmHg) | 20 | 20
|
5.3 What do these findings indicate?
Case 6:
(Click here to go to the answers)
On Friday, December 13, 1799, George Washington, recently retired as 1st President of the United States, developed a "cold" with mild hoarseness, but by 2 am the next morning he had difficulty breathing, with fever, throat pain, and difficulty swallowing. He was given the usual treatment of the time--bloodletting, with removal of about 400 mL. The first physician to arrive at 9 am, Dr. James Craik, supervised blistering agents applied to his throat, to draw off "toxins". Another 500 mL of blood was removed. An additional 500 mL of blood was removed at 9:30 am. He was given vinegar to gargle, which led to near fatal choking. Washington was still able to walk about his bedroom. Another physician, Elisha Dick, arrived and advised against further bloodletting, but another 1000 mL were removed at 3 pm. Dr. Gustavus Brown arrived and supervised administration of calomel (mercurous chloride) and tartar emetic (antimony potassium tartrate) as purgatives. Though Washington's condition temporarily improved, by 8 pm he was in greater respiratory distress. Further blistering agents were applied. Washington died at 10:20 pm.
Had vital signs been recorded, they may have shown temperature 37.9 C, pulse 115/min, respiratory rate 24/min, and blood pressure 90/60 mm Hg supine and 80/40 mm Hg sitting. An arterial blood gas may have shown pH 7.43, pO2 92 mm Hg, and pCO2 38 mm Hg with O2 saturation of 96%. His Hgb was 6.8 g/dL with Hct 18.2%, MCV 92 fL, platelet count 246,000/microliter, and WBC count 7720/microliter.
Questions:
6.1 What is his calculated O2 content?
6.2 What key factors affect this measurement? How could it have been improved in this case?
6.3 What physiologic changes occurred as a consequence of bloodletting and purging?
Case 7:
(Click here to go to the answers)
A 101-year-old healthy woman with no major medical problems except for osteoarthritis has a fainting episode. She is taken from a nursing home to the emergency department. Vital signs show T 37 C, P 80/min, RR 18/min, and BP 135/90 mm Hg. Her lungs are clear to auscultation and heart rate regular with no murmurs. A chest radiograph shows a normal cardiac shadow, no infiltrates, but there are a few small left upper lobe bright densities, brightness of the aortic arch, and brightness of small muscular arteries in the lower neck region. An arterial blood gas shows pH 7.42 pO2 79 mm Hg, pCO2 40 mm Hg, and O2 saturation 90% on room air.
Questions:
7.1 Calculate her A-a (alveolar - arterial) oxygen gradient. What key factors affect this measurement?
7.2 If the A-a gradient is normal but the PaCO2 is increased, what is suggested?
7.3 If the A-a gradient is increased, and the PO2 decreased, what is the explanation?
7.4 If the A-a gradient is normal, but the PO2 is decreased, what is the explanation?
Case 8:
(Click here to go to the answers)
A 3-year-old child is noted by her mother to have developed a funny grayish-blue skin tone over the past day. The child passes brown urine. The child is taken to the emergency department. Vital signs show T 37.1 C, P 100/min, RR 31/min, and BP 90/60 mm Hg. The physican assistant auscultates clear lungs, and the heart rate is regular with no murmurs. There are no remarkable findings except for the odd steel gray skin colour. A pulse oximetry measurement reveals an oxygen saturation of 75%. Laboratory studies show Hgb 13.1 g/dL, Hct 39.5%, MCV 93 fL, platelet count 199,950/microliter, and WBC count 6620/microliter. Her serum glucose is 75 mg/dL and creatinine 0.4 mg/dL. Adminisitration of 5L of oxygen by face mask does not improve the child's skin colour. An arterial blood gas shows pH, 7.43, pO2 285 mm Hg, pCO2 32 mm Hg, and oxygen saturation 99%. The technician doing the radial arterial puncture notes an odd brown colour to the blood in the syringe.
Questions:
8.1 What is suggested by these findings?
8.2 Explain the biochemistry behind this phenomenon.
8.3 What caused this problem?
8.4 Explain the use of pulse oximetry
Case 9:
(Click here to go to the answers)
A 30-year-old injection drug user develops a high fever and chills. On examination vital signs show temperature 39.2 C, pulse 115/min, respiratory rate 20/min, and blood pressure 80/50 mm Hg. Auscultation of the chest reveals a holosystolic murmur at the lower left sternal border. The intensity of the murmur increases with inspiration. Observation of the neck veins reveals the following venous pulsations
Questions:
9.1 What do these findings indicate?
9.2 What additional studies should you do?
Additional history:
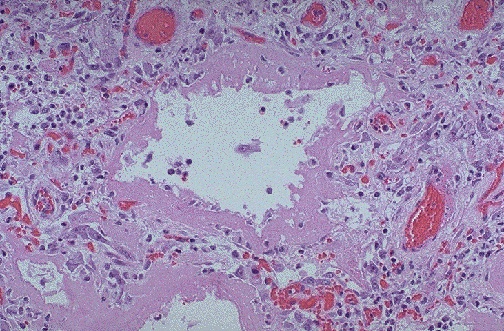
He undergoes emergent surgery with tricuspid valve replacement. He receives antibiotic therapy with ticaracillin and tobramycin. A repeat blood culture shows no growth. He requires supplemental oxygen with an FI02 of .80. Examination of the lungs shows crackles bilaterally. He has tachycardia without an S3 gallop. Chest roentgenogram reveals diffuse infiltrates in both lung fields with an alveolar pattern.
He now has the following hemodynamic pressure measurements:
| Arterial BP | 105/70 mm Hg
| | RA (CVP) | 8 mm Hg
| | PA | 60/32 mm Hg
| | PAWP | 10 mm Hg
| | HR | 106/min
|
9.3 What is suggested by these findings?
9.4 If his left chamber volume at end of diastole = 0.12 L, chamber volume at end of systole = 0.07 L, and he is an average-sized person with a body surface area of 1.62 m2, calculate his cardiac output, cardiac index, and ejection fraction.
9.5 What is DLCO and what would you expect it to be in this case?
Return to the Main Menu
|