|
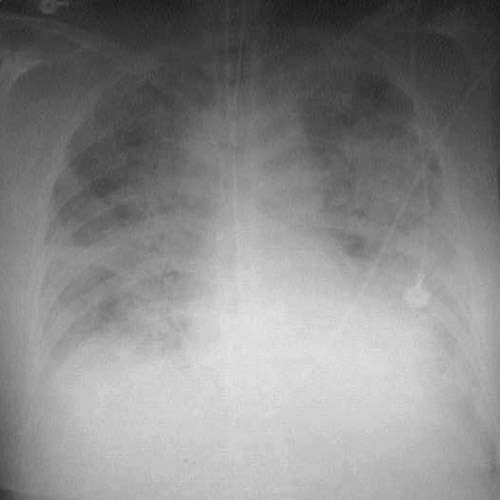
A 74-year-old man has experienced substernal chest pain for the past 3 hours. The pain is constant. He is now becoming short of breath. In the emergency department his vital signs include temperature 37.1 C, pulse 108/min, respiratory rate 29/min, and blood pressure 90/70 mm Hg. He is unable to lie supine. Auscultation of the chest reveals bilateral crackles in lower lung fields. He has a summation (S3 and S4) gallop. A chest radiograph shows prominent bilateral perihilar infiltrates.
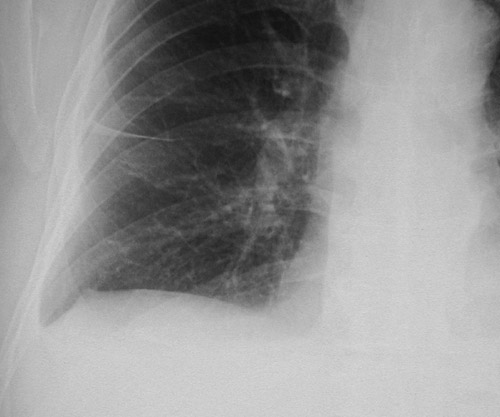
Example 1:

Example 2:
Example 3:
Questions:
4.1 What is suggested by these findings?
Acute myocardial infarction with pulmonary edema
4.2 What tests would help confirm the diagnosis?
His total CK is 332 U/L with CK-MB fraction of 8%. His troponin I is 10 ng/mL.
Additional history:
He is admitted to the hospital. He receives thrombolytic therapy with tPA. His condition is stable. He receives pharmacologic therapy with an anticoagulant, probably a low moleculart weight heparin analogue. Other possible therapies include an anti-platelet agent or a beta-blocker.
He now has the following hemodynamic pressures:
| Arterial BP | 100/75 mm Hg
| | RA (CVP) | 12 mm Hg
| | PA | 36/28 mm Hg
| | PAWP | 28 mm Hg
| | HR | 115/min
|
4.3 What do these findings indicate?
Acute pulmonary edema.
4.4 If his left chamber volume at end of diastole = 0.11 L, chamber volume at end of systole = 0.08 L, and he is an average-sized person with a body surface area of 1.62 m2, calculate his cardiac output, cardiac index, and ejection fraction.
Stroke Volume = ((Chamber Volume at End Diastole) - (Chamber Volume at End Systole)) = 0.03 L
Cardiac Output = (Stroke Volume) X (Heart Rate) = 3.45 L/min
Cardiac Index = (Cardiac Output) / (Body Surface Area) = 2.13 L/min/m2
Ejection Fraction = ((Stroke Volume) / (Chamber Volume at End Diastole)) * 100 = 27%
| 


