|
A 44-year-old man participates in a health screening program and is found to have a blood pressure of 166/106 mm Hg. He goes to a physician who finds no abnormalities on physical examination. Laboratory studies show sodium 140 mmol/L, potassium 3.9 mmol/L, chloride 104 mmol/L, CO2 25 mmol/L, glucose 93 mg/dL, creatinine 1.4 mg/dL and urea nitrogen 32 mg/dL. A urinalysis shows pH 6.5 with sp gr 1.018, and no blood, protein, glucose, or ketones. Urine electrolytes show sodium 15 meq/L and osmolality 600 mosm/L.

An abdominal ultrasound shows normal sized kidneys without dilation. The length between the markers is about 12 cm.
He is placed on an angiotensin converting enzyme (ACE) inhibitor. A week later he develops increasing nausea, headache, and oliguria. He takes ibuprofen for the headaches. His condition does not improve.
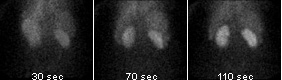
Below is a normal renal scan, with intravenous administration of Tc-99m (a radionucleide), following by timed images.
In the following study, the patient had a renal scan performed priorto administration of intravenous enalapril:
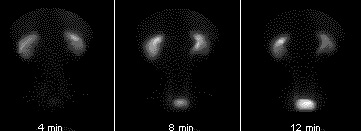
In the following study, the patient had a renal scan performed after administration of intravenous enalapril:
Following administration of the ACE inhibitor, there is marked asymmetry in renal function, with normal uptake and excretion by the right kidney but little or no excretion on the left. This test is a good screening tool for renovascular hypertension.
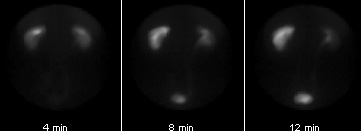
Another study is performed, as shown below:

Questions:
2.1 Explain what may have happened?
His hypertension is due to renal vascular constriction on the left, typical for renal arterial atherosclerosis with narrowing. When there is reduced renal blood flow, GFR is maintained by prostaglandin-mediated relaxation of afferent arterioles and by angiotensin II mediated efferent arteriolar constriction. The ACE inhibitor will decrease efferent arteriolar tone and decrease the glomerular capillary perfusion pressure. Non-steroidal anti-inflammatory drugs (NSAIDs) will inhibit prostaglandin synthesis and lead to vasoconstriction that diminishes the renal blood flow and GFR. Thus, the drugs this man took exacerbated his renal failure.
His creatinine has increased to 4.1 mg/dL, with urea nitrogen of 44 mg/dL.
Urine electrolytes now show sodium 49 meq/L and osmolality 290 mosm/L
2.2 Explain the progression of his disease?
The drug-induced renal vasoconstriction has resulted in renal injury, probably involving tubules, with acute tubular necrosis. Thus, the urine electrolytes, the osmolality, and the BUN/Cr ratio suggest intrinsic renal disease, whereas the initial values suggested prerenal azotemia.
2.3 What pharmacologic therapy should he have initially received?
A beta-blocker plus a diuretic would have been more appropriate. His headaches (if he still experienced them, or episodic headache) could have been relieved with acetaminophen, which has little effect upon renal prostaglandins.
2.4 What can be done next?
Surgery with resection of the stenotic portion of left renal artery and placement of a graft can be performed.
| 


