|
A 35-year-old man has had diarrhea with a 5 kg weight loss over the past year. On physical examination there are no abnormal findings. Laboratory studies show Hgb 13.5 g/dL, Hct 40.6%, MCV 89 fL, platelet count 241,000/microliter, WBC count 5580/microliter, sodium 142 mmol/L, potassium 4.0 mmol/L, chloride 110 mmol/L, CO2 22 mmol/L, glucose 72 mg/dL, creatinine 0.9 mg/dL, amylase 30 U/L, total protein 5.8 g/dL, albumin 3.7 g/dL, AST 28 U/L, ALT 19 U/L, alkaline phosphatase 77 U/L, and total bilirubin 1.0 mg/dL.
Questions:
7.1 What diagnoses may be considered?
It is unlikely that an infectious diarrhea would last that long. Congenital conditions such as cystic fibrosis are unlikely, though lactase deficiency may be considered. Celiac sprue is a possibility. Pancreatic and biliary tract disease are unlikely to be silent, without abdominal pain. Inflammatory bowel disease is more likely to produce more severe and episodic symptoms. Could it be diet-related?
7.2 What else do you want to know?
When asked about the nature of the diarrhea, he says that he can have 8 to 12 stools a day, sometimes 2 to 5 times per week. The stools are watery but not bloody. He had a similar chronic diarrheal condition about 2 years ago, which lasted for 6 months. He has tried changing his diet from hi-carb to low-carb to more fiber to less fiber to more frequent meals to less frequent meals, to more alcohol to no alcohol, all without any apparent difference in symptoms.
7.3 What diagnostic tests can be done?
| Quantitative stool fat | 8 gm/day
| | Stool for occult blood | negative
| | Stool for ova and parasites | negative
| | Urinary d-xylose | decreased
|
Upper GI endoscopy is performed. There are no esophageal or gastric lesions; duodenum shows slight erythema; jejunum shows loss of mucosal folds and erythema.
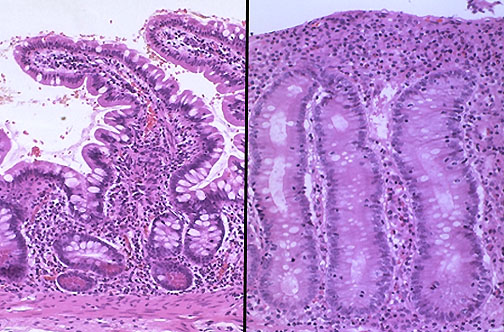
Jejunal biopsy has the microscopic appearance shown at the right (compared with normal at the left), with loss of villi, flattening of villi, increased inflammation, and diminished goblet cells.
7.4 What is the diagnosis?
Celiac sprue.
7.5 What is the cause for this? What is the mechanism for the diarrhea?
The small bowel mucosa becomes inflamed, with flattening and blunting of villi. There are genetic, environmental, and immunologic factors. About 95% of patients have the HLA-DQ2 allele. The disease is more common in Caucasians and uncommon in Blacks and Asians. The key environmental factor is dietary gluten in wheat, barley, oats, and rye, with the protein gliaden. Anti-gliaden and antiendomysial antibodies (of the IgA type) can be found in over 90% of cases.
The diarrhea is in part due to malabsorption of fats with steatorrhea. This can be due to diminished jejunal absorption. There is decreased lactose digestion. There is increased mucosal fluid production. There is bile acid malabsorption with bile acid-induced colonic mucosal secretion.
7.6 What is the treatment?
He requires a gluten-free diet. Decreasing his intake of fats and milk products can help as well.
7.7 What are complications?
There is an increased risk for gastrointestinal lymphoma. Some patients have additional immunologically mediated conditions, including type I diabetes mellitus and dermatitis herpetiformis.
7.8 Outline the absorption mechanisms for carbohydrates, fats, and proteins.
Carbohydrates:
Starches can be broken down by salivary gland and pancreatic amylase to dextrin and to maltose. These are digested to glucose by dextrinase and maltase.
Sucrose (glucose + fructose) is broken down by small bowel sucrase.
Lactose (glucose + galactose) is broken down by small bowel lactase.
Fats:
Lingual and gastric lipases can break down triglycerides to fatty acids and glycerol.
Pancreatic lipase breaks down triglycerides to fatty acids and monoglycerides.
Pancreatic phopholipases break down phospholipids to fatty acids.
Bile helps emulsify fats to smaller droplets (micelles) for more surface area action by lipases.
The cholesterol, monoglycerides, lecithin, and free fatty acids are absorbed into enterocytes, where they are reprocessed to triglycerides, cholesterol, and phospholipids that are complexed with apoproteins to form chylomicrons in the Golgi apparatus. The chylomicrons are dumped into villus lacteals.
Proteins:
Gastric pepsin helps cleave peptide bonds to form polypeptides.
Pancreatic peptidases break down proteins and polypeptides to amino acids. Pancreatic enzymes are secreted as inactive precursors: trypsinogen, chymotrypsinogen, proelastase, procarboxypeptidases A and B. These are activated by enterokinase from enterocyte microvilli, producing trypsin that activates all of them.
Small bowel mucosal peptidases break down proteins and polypeptides to amino acids.
Pancreatic ribonuclease and deoxyribonuclease break down RNA and DNA to nucleic acids.
Vitamins:
The fat soluble vitamins A, D, E, and K are absorbed with lipids and packaged with the chylomicrons. The water soluble B and C vitamins are absorbed via a sodium-dependent cotransporter in enterocytes.
Vitamin D (cholecalciferol) is converted to 25-hydroxycholecalciferol in liver and to the active 1,25 dihydrocholecalciferol in kidney which induces enterocyte synthesis of calbindin to promote calcium absorption.
|



