|
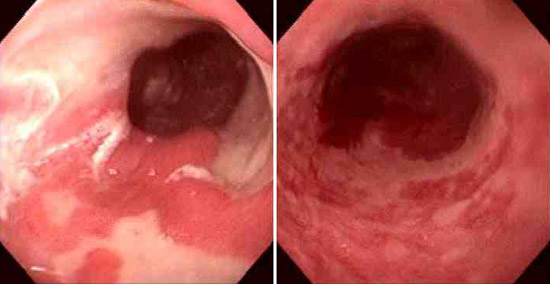
A 51-year-old man has been bothered by chest pain for the past 20 years. He describes the pain as dull and burning. On physical examination there are no abnormal findings. Upper GI endoscopy shows the findings seen here:
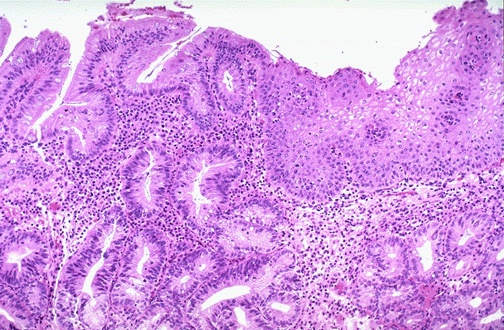
A biopsy shows the microscopic finding seen here:
Questions:
4.1 What is the diagnosis?
GERD with Barrett mucosa.
4.2 What is the pathophysiology of this condition? What condition is the opposite of this one?
The lower esophageal sphincter (LES) normally maintains tonic activity from acetylcholine release from vagal nerves. When the LES tone diminishes, it fails to prevent reflux of acid contents into the lower esophagus. When this occurs on a chronic basis, there is inflammation of the non-keratinizing stratified squamous epithelium of the lower esophagus. There can be columnar metaplasia in response to the continued inflammation. Potential complications include ulceration and stricture. Persistence of the condition for many years increases the risk for epithelial dysplasia that can progress to adenocarcinoma.
The opposite condition is achalasia, in which there is failure of relaxation of the LES. There is a deficient myenteric plexus with diminished nitric oxide and VIP production.
4.3 What pharmacologic therapy is available? How does it work?
Gastric acid secretion occurs when parietal cells produce hydrogen ion. Acid secretion is stimulated by ingestion of peptides and amino acids, gastric distension from ingested food, and from vagal stimulation after seeing and smelling food, all leading to release of "little" gastrin from G cells in the stomach mucosa.
Proton pump inhibitors such as omeprazole (and H2 receptor blockers such as famotidine) reduce the acidity of the gastric contents and thus reduce further mucosal damage to the esophagus. Though these drugs do not reverse the damage already done, diminished acidity may allow healing and reversal of the metaplasia (Barrett mucosa).
Antacids can reduce pain of either GERD or peptic ulcer disease by reducing the acidity.
Metoclopramide (Reglan ®) has several actions upon motility. It increases antral contractions, relaxes the pyloric sphincter, and increases duodenal and jejunal peristalsis. This leads to faster gastric empyting and bowel transit. Metocloprromide increases the lower esophageal sphincter (LES) tone to reduce reflux into the lower esophagus. Since metoclopramide increases gastric emptying, it is useful in treating diabetic gastroparesis.
| 


