|
A 34-year-old woman has noted intermittent but sharp abdominal pains for the past 2 days. On physical examination her vital signs include T 37 C, P 83/min, RR 18/min, and BP 140/90 mm Hg. Her lungs are clear to auscultation and her heart rate is regular with no murmurs. She has right upper quadrant tenderness on palpation. Bowel sounds are active. Her stool has no detectable occult blood. Laboratory studies show Hgb 11.8 g/dL, Hct 36.0%, MCV 121 fL, WBC count 9200/microliter, platelet count 262,000/microliter, glucose 66 mg/dL, creatinine 0.9 mg/dL, amylase 22 U/L, AST 44 U/L, ALT 25 U/L, total bilirubin 1.0 mg/dL, and alkaline phosphatase 69 U/L.
Questions:
3.1 What do you suspect and what studies would you perform?
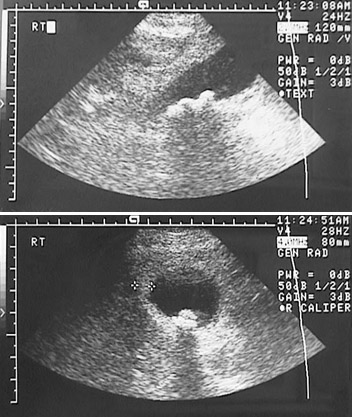
Acute cholecystitis. The simplest initial study is abdominal ultrasound, which shows multiple gallstones. There is no evidence for common bile duct or pancreatic duct obstruction, but cholangiography would help to demonstrate such a finding.
Additional history:
She has had bouts of abdominal pain for the past 7 years. These bouts have lasted from 1 to 4 weeks on average, accompanied by diarrhea.
3.2 What is suggested by these findings?
This could be cholecystitis, but it may be something else, such as an inflammatory bowel disease. An abdominal CT scan is performed:
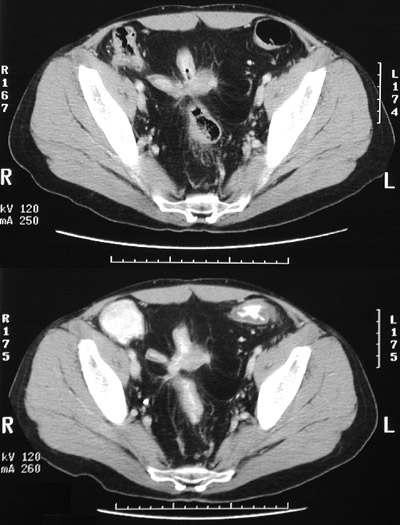
The CT shows focal thickening of loops of ileum with narrowing of the lumens and adhesions with fistulae between loops. This is more consistent with Crohn disease than ulcerative colitis. A colonoscopy is performed and shows no colonic lesions.
3.3 How does this explain the initial findings above?
Involvement of the terminal ileum with Crohn disease can lead to malabsorption. There is an enterohepatic circulation of bile salts. Over 90% of the bile salts excreted with the bile are reabsorbed in the terminal ileum via the enterocyte sodium-bile salt cotransporter. Bile formed in the liver contains the bile salts cholic acid and chenodeoxycholic acid. Gut bacteria convert these to deoxycholic acid and lithocholic acid. The bile salt pool is about 3 g, and the liver produces about 0.5 g/day to replace that lost in the intestine, but cannot markedly increase bile salt production to compensate for greater intestinal loss. The disturbed enterohepatic circulation leads to an alteration in the composition of the bile that favors calculus formation, because the relative concentrations of bile salts, lecithin, cholesterol, and bilirubin are altered.
In addition, vitamin B12 (cobalamin) complexed to intrinsic factor is absorbed in the terminal ileum. In this case, the diminished absorption of B12 has resulted in a megaloblastic anemia.
The pain of cholecystitis occurs when a stone impacts in the neck of the gallbladder or travels down the cystic duct or into the common bile duct. The passage of chyme with peptides and fatty acids from the stomach into the duodenum stimulate mucosal endocrine cells to secrete cholecystokinin (CCK) which stimulates gallbladder contraction. Thus, the pain of cholecystitis may be episodic and related to eating foods with a high protein and fat content.
3.4 What if this patient's total bilirubin had been 3 mg/dL? Explain bilirubin metabolism.
An elevated bilirubin can occur from biliary tract obstruction from the common bile duct to the ampulla of Vater, from an overproduction of bilirubin, or hepatic dysfunction. Measuring the direct bilirubin gives a indication of the possible etiology.
Breakdown of hemoglobin generates bilirubin, which circulates bound to albumin and is known as "unconjugated" or "indirect" bilirubin. This indirect bilirubin is taken up into hepatocytes and bound to cytoplasmic proteins. The smooth endoplasmic reticulum enzyme uridine diphosphate glucuronyl transferase causes a bilirubin molecule to combine with two molecules of uridine diphosphate (UDP) glucuronic acid, forming bilirubin diglucuronide, the "conjugated" form that is water soluble and excreted into the bile canaliculi. However, some bilirubin diglucuronide "leaks" into the circulation and is excreted by the kidney into urine.
An overproduction of bilirubin from breakdown of RBCs (hemolysis) leads to an increase mainly in the indirect component. Biliary tract obstruction leads to an increase mainly in the direct component. Hepatic dysfunction is marked by an increase in both.
| 


