|
A 24-year-old woman is in the third trimester of her first pregnancy. There have been no problems, with fundal height consistent for gestational age. She goes into labor and begins hemorrhaging profusely. She is taken to the hospital, and on admission has vital signs with T 36.8 C, P 116/min, RR 22/min, and BP 80/40 mm Hg. Her skin is cool and clammy. She has marked vaginal bleeding. An abdominal ultrasound shows a low-lying placenta. The fetus is viable, with heart tones from 140 to 150/min. Laboratory studies show Hgb 6.4 g/dL, Hct 19%, MCV 80 fL, platelet count 207,300/microliter, and WBC count 5920/microliter.
Questions:
2.1 What is the diagnosis?
She has placenta previa.
2.2 What should be done next?
An emergent cesarean section. A normal 3100 gm term female baby is delivered. Her hematocrit is 18%. She needs a transfusion. A type and cross is performed and 2 units of packed RBCs are given. Her post transfusion, post C-section hematocrit is 24%.
Additional history:
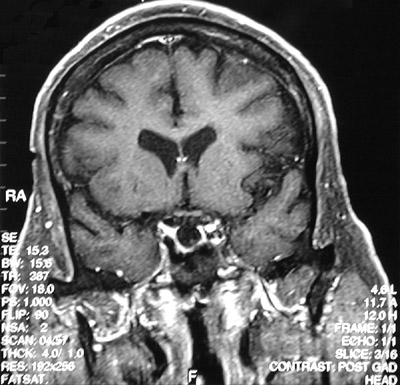
A month following delivery she is unable to nurse the baby. She has increasing polyuria and polydipsia. She then has a fainting episode. MR imaging of the head reveals the following:
2.3 Explain these findings.
She has Sheehan syndrome (pituitary apoplexy). Note the absence of tissue density within the sella turcica. The posterior pituitary hormones, including oxytocin and vasopressin (antidiuretic hormone) are deficient, with failure of lactation and development of diabetes insipidus. During pregnancy, the pituitary enlarges slightly, which makes the pituitary blood supply more tenuous, and the hypotension with blood loss during delivery exacerbates the ischemia. In general, about 90% of the pituitary must be destroyed to result in significant loss of function.
Laboratory studies show Hct 30%, sodium 129 mmol/L, potassium 5.0 mmol/L, chloride 89 mmol/L, CO2 19 mmol/L, glucose 60 mg/dL, and creatinine 1.0 mg/dL.
These findings are consistent with acute Addison disease from the loss of ACTH and diminished mineralocorticoid and glucocorticoid production.
2.4 If she is not treated at this point, what could happen?
FSH-LH deficiency leads to loss of menstrual cycles and infertility. ACTH is the next anterior pituitary hormone to become deficient, followed by TSH and hypothyroidism. The acute Addison disease is the rate-limiting step to survival.
2.5 What is the treatment?
She requires hormone replacement therapy:
Mineralocorticoid and corticosteroid replacement are accomplished by giving fludrocortisone (Florinef ®). A dose equivalent to 20 mg in the morning and 1/3 to 1/2 that dose in the evening is typically sufficient. The dose must be increased if increased stress (such as a surgical procedure--or a visit by relatives--is anticipated.
Additional replacements may include:
Estrogen
Progesterone
L-thyroxine
Somatotropin
Vasopressin
| 


