Background: Embolism is defined as the obstruction of a blood vessel by a clump of material, such as a broken-off piece of plaque, a blood clot or air bubble, travels through the bloodstream and becomes lodged in a blood vessel. Depending on the size of the embolism and which blood vessel it is obstructing, the result can range from no symptoms whatsoever to a life-threatening emergency.
the overriding interest in clinical practice is defining the risk that a given pathological situation or a cardiovascular device can lead to. Objectives: In this study, it was hypothesized that by differentiating well-defined flow patterns, such as jet flow and circulation zones, and by controlling their dominant geometrical values, a data on the generation rate of thromboembolism can be provided.
Methods: The study is conducted in three consecutive stages:1. A modular in-vitro flow loop for the implantation of the models that circulated platelet rich plasma (PRP). 2.A custom made light scattering microemboli detector (LSMD) device that could count and measured the emboli size. 3. Digital Particle Image Velocimetry (DPIV) measuring system was used to map the flow field in models similar to those used in the in-vitro flow loop.
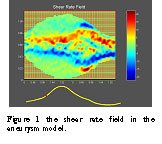
The flow cells in the experiment were chosen as follows: big aneurysm, small aneurysm, 65% area reduction tube and a control, Figure 1 shows the inverse model of the aneurysm model (the lumen). The ratio between the tube diameter to the aneurysm diameter for each model are 2.8, 2.2, which is the smallest.

Figure 1: The aneurysm models
As aforesaid, the main hemodynamic factors, shear stresses and residence time, were modeled using constriction and circulation flow cells. The flow values were related to those in the main cerebral arteries, since both extreme hemodynamic states causing from stenosis and aneurysm commonly occur at those arteries as shown in Table 1.
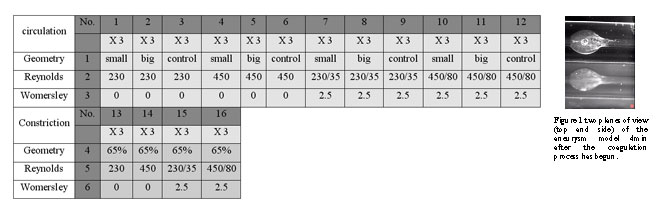
Table 1: Experiment table
Preliminary results & discussion: the results form the in-vitro PRP flow loop have shown that by using the LSMD through the process of coagulation five consecutive stages can be distinguished as follows (Figure 2):
Figure 3 shows two planes of view (top and side) of the deposition region in the big aneurysm model (Indicated as no.11 in Table 1) after 4 min from the initiation of the coagulation cascade. It can be seen that the platelets begin to deposit few millimetre distally to the aneurysm and proceed to deposit upstream. Figure 4 depict the shear rate field of the same model demonstrated in Figure 3 The shear rate at the beginning of the systolic phase increased dramatically at the distal neck of the aneurysm.
A thrombus, as noted previously, is the final product of the coagulation cascade, in which the free passage of the blood stream is interacting with the coagulation reaction to vessel injury or blood flow abnormality. The initiation of that process, from the biomechanical point of view, relates to the activation of the platelets due to blood flow abnormality. Those biomechanical factors elicit a cascade of biochemical factors (procoagulants) that initiate the formation of a thrombus, which will eventually be released as thromboemboli.
More specifically, two extreme flow patterns play a major role in the initiation of the coagulation cascade: low shear rates combined with long residence time and high shear stress combined with short residence time. Once the platelets have been activated, they were convected with the other formed elements in the PRP and, depending on the details of the local flow field; they have the potential to accumulate in certain regions as indicated in figure 3.
In addition to low shear stresses found in the aneurismal region, the circulation value represented
the rate at which the coagulation mediators bind together and enhance the coagulation process. The other suggested model was that of a constricted flow cell that increased the shear stress in the flow loop. The flow parameters governed in that case, i.e., the reduction of the lumen area determined the increase in shear stresses and the length of the constriction determined the duration of exposure to the stresses. In our preliminary work, the averaged shear stresses inside the constricted area exceeded the value known in the literature as being the critical value to initiate the generation of a thrombus and showed an increase in the formation of thromboses.
Finally, further examination of the flow characteristics that lead to thrombus formation resulting from typical geometries may contribute useful clinical information for risk evaluation stemming from either pathologies or bioprosthesis devices.
