Background: The importance of arterial revascularization raises the question whether the use of the internal thoracic artery (ITA) should be extended to its sub-divisions. The aim of the present in vitro study is to compare the vascular reactivity and morphology of the distal ITA and its branches, the Superior Epigastric (SE), and Musculophrenic (MP) arteries, and to analyze the effect of patientís characteristics on the active response.
Methods: Active response of 122 skeletonized arterial rings obtained from 55 consecutive patients undergoing CABG was investigated in organ baths. Normalized physiologic passive conditions were determined based on a length-tension curve obtained for each individual ring. Cumulative doses of Norepinephrine NE (10-9-10-4 M) were added to create a dose-response curve. The maximal response and sensitivity (EC50) were statistically analyzed according to age, gender, risk factors, medications and different sites of the ITA, applying multivariant analysis to assess their influence on reactivity. Histological studies included H&E, elastic fibers and smooth muscle actin stains.
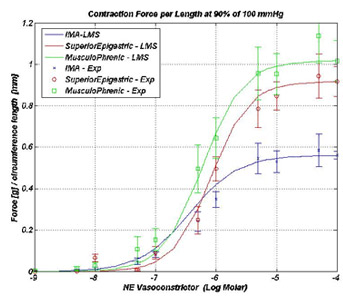 Results: The distal ITA is significantly less reactive to NE than its subdivisions (p~0.005). No significant difference was noted between SE and MP (p=0.28) -see figure. There is a trend of decreased reactivity with increasing age (p=0.095), but reactivity is similar between genders. Regarding medical therapy: patients treated with beta blockers have a significantly decreased reactivity (p=0.009). Alpha blockers have the same effect but didnít reach significance after adjusting to age. Analysis of risk factors failed to pinpoint a single factor which may affect reactivity.
Results: The distal ITA is significantly less reactive to NE than its subdivisions (p~0.005). No significant difference was noted between SE and MP (p=0.28) -see figure. There is a trend of decreased reactivity with increasing age (p=0.095), but reactivity is similar between genders. Regarding medical therapy: patients treated with beta blockers have a significantly decreased reactivity (p=0.009). Alpha blockers have the same effect but didnít reach significance after adjusting to age. Analysis of risk factors failed to pinpoint a single factor which may affect reactivity.
Histological analysis on 16 patients revealed minimal intimal hyperplasia in all patients. One patient had significant atherosclerosis. Quantitative analysis aimed at correlating the degree of muscularity with reactivity in ITA, SE and MP is under investigation, and will be presented.
Conclusion: When planning the revascularization procedure, surgeons should consider the greater reactivity in the distal ITA and its subdivisions, especially in young patients not treated with adrenergic blockers. The significance of these findings should be further evaluated in clinical studies.
