Background: Previous work, using various lasers and various "biological glues", has shown laser soldering to be an effective method for connecting blood vessels, peripheral nerves, parts of the urinary tracts and the intestine. These glues (and not the underlying tissue) are activated by laser beams and they act to join the tissues together. Laser soldering has been tried in gynecology, otolaryngology and microsurgery. Limited clinical trials have shown laser welding (without solder) to be as strong as suture techniques with much less histological evidence of local inflammation. The mechanisms by which laser tissue welding (LTW) and soldering (LTS) are contributing to wound healing and closure are not yet fully understood. One reason for the difficulty in applying the experience gained in these research works to general clinical practice is the inconsistency of the experimental results. Studies by different groups reported a wide range of methods and conditions under which bonds are formed. Most studies cite only a subjective change in the welded tissue characteristics (such as blanching, browning or shrinking) as an end point for the welding process. These studies reported the laser energy used, but often failed to report the more relevant factor: the temperature achieved in the laser-irradiated tissue. Biological effects in tissue depend exponentially on temperature T and linearly on time t. Small temperature changes cause large changes and may lead to no welding at low T (e.g. 30
0C) or to necrosis at high T (e.g. 100
0C). In both cases the strength of the bonded cut was low. There is only a narrow temperature range where tissue soldering is expected to be efficient. Our goal has been to develop a system that will monitor and control the temperature of the soldered cut within the narrow range around 60-80
0C, thus leading to reliable and strong bonding.
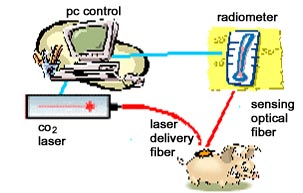
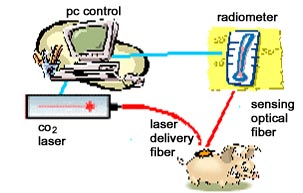
Hypothesis: In principle, laser soldering may close cuts in the tissue, providing strong and watertight bonding, without leaving scars. The quality of the bond must depend on the temperature T at the soldering site, but temperature measurements of laser irradiated tissue are difficult to perform and have led to conflicting and unreliable results. Infrared (IR) emitted from a body depends on its temperature T. Thus a non-contact radiometric measurement of the IR emissions can be used to determine T. Fiberoptic IR radiometry provides a means of accurate, noncontact temperature measurement of laser-irradiated tissues. Our hypothesis was that with such a fiberoptic system, based on unique fibers developed at Tel Aviv University, we would be able to obtain strong and reliable bonding. Our hypothesis was that this would be very useful for bonding of blood vessels, including microvessels.
Experimental Results: Utilizing this method for the monitoring and control of CO
2 laser irradiated tissue, we achieved good temperature control during tissue heating. Using the fiberoptic system, we carried out soldering of various tissues in vivo and
in vitro. The preliminary results, obtained mostly for thin tissues, have been very encouraging. In particular we have successfully used the laser soldering system for bonding of blood vessels in rats and rabbits, in vivo. Experiments are being planned now for the anastomoses of blood vessels in larger animals (e.g. pigs).
Conclusions: A fiberoptic laser soldering system makes it possible to obtain strong and reliable bonding between tissues. This work will lead to the clinical use of laser soldering in the cardiovascular system. It should be emphasized that this bonding technique lends itself easily for endoscopic applications, which may be useful for example for least invasive heart surgery.